Breast Augmentation

Breast augmentation is a cosmetic surgery procedure designed to enhance the body contour of a woman unhappy with her breast size. It may also be used to correct volume loss after pregnancy, or to help balance breast size asymmetries, as well as a reconstructive technique following another breast surgery procedure such as mastectomy.
While breast augmentation will enlarge the breasts, it will not alter basic defects in breast shape or form. Major asymmetries may be improved, but will not be completely corrected. A slight difference in the size or shape of the two breasts is considered normal and should not be a cause for concern. If breast size or nipple position asymmetries are severe then additional procedures to further improve symmetry may be necessary. Long experience with this operation has demonstrated it to have highly satisfactory results for the majority of patients who are considered suitable candidates for the surgery.
Whether you are looking for breast augmentation (silicone implants or saline implants), a breast lift, breast reduction or other breast enhancement surgery, Chugay Cosmetic Surgery offers a variety of options to help you look your very best.
We utilize state-of-the-art techniques to deliver aesthetically pleasing and natural looking breasts.
Breast Augmentation Incisions
At Chugay Cosmetic Surgery, we offer three primary incisions for breast augmentation:
- Nipple areolar complex (at the border of the areola)
- Inframammary fold (in the crease of the breast)
- Axillary (in the armpit)
At the time of your consultation, your surgeon will discuss which options are best suited for your skin type and will offer some advice as to which incision best suits your needs.
Breast Implants
Currently, there are two types of implants available for augmentation. Regardless of the implant that you choose, beautiful results can be had with both types of implants. At the time of your consultation, you will have the opportunity to feel both types of implants and discuss the two options with your surgeon in order to find the best option for you.
Silicone breast implants
Silicone implants were first popularized in the 1960’s. Controversy in the early 1990’s led to widespread fear about the possibility of silicone breast implants causing autoimmune diseases in women or possibly linked to cancer development. Extensive studies since then have showed no evidence that silicone breast implants have any relationship to breast cancer, autoimmune disease or any other systemic illnesses in patients. Specifically, patients with breast implants have no higher incidence of diseases such as rheumatoid arthritis, scleroderma or lupus, in comparison with the general population.
The Food & Drug Administration approved the use of the third generation silicone gel implants in November of 2006. These implants are not filled with liquid silicone, but rather a cohesive silicone gel. The increased safety of the cohesive gel implants led to the FDA’s approval of these implants for cosmetic use.
Silicone implants tend to feel more natural and have a lesser chance of rippling. However, on the other side of the coin they are a bit more costly and have a higher chance of producing a thickening of scar tissue around the implant known as capsular contracture.
Saline breast implants
Saline implants are implants that are filled with sterile salt water. They are very safe and if they become damaged or deflate, your body will absorb the water. Saline implants are more prone to rippling and feel less natural than silicone.
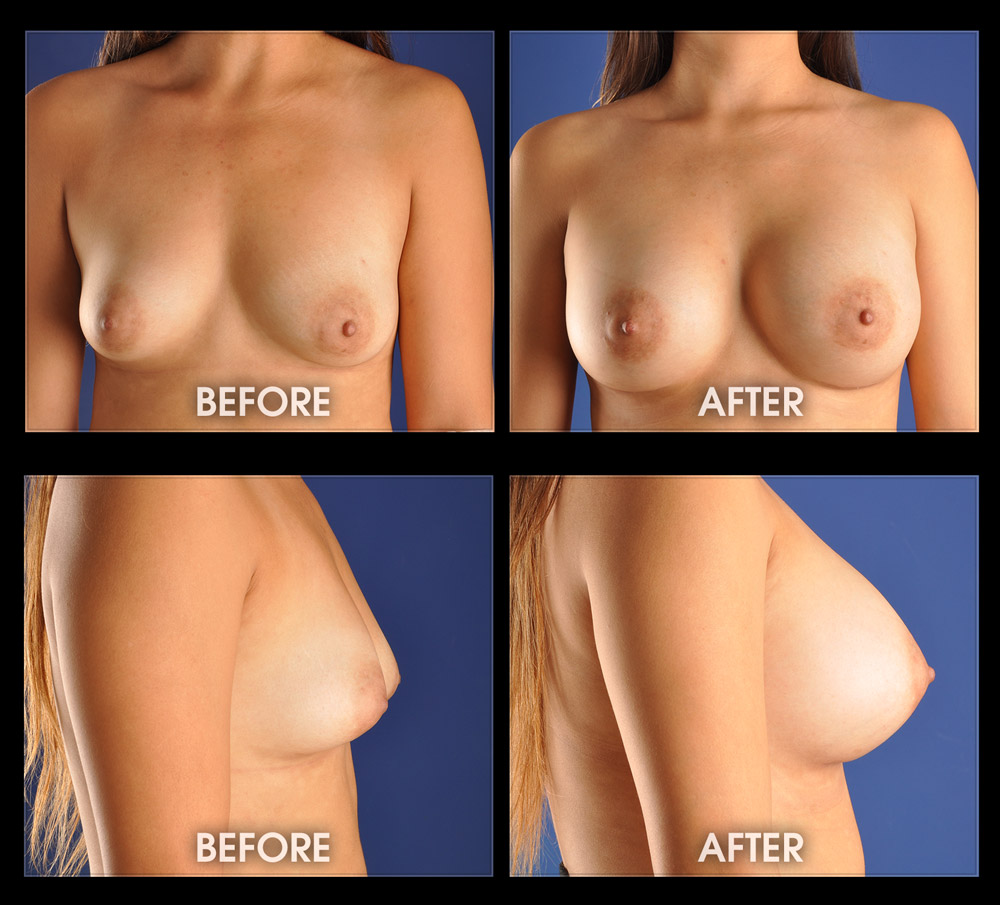
*INDIVIDUAL RESULTS WILL VARY. IMAGES DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
Common Questions / Concerns
How will I Care for My Implants After Surgery?
Patients are asked to wear a compression bra after surgery to help limit swelling and lock the implants in the desired position. We ask all patients to begin laying on their chest at 2 weeks to help stretch out the capsule that is forming around the implant. This will help to possibly prevent a case of capsular contracture.
Following breast augmentation patients will need to continue routine breast screening with their primary care physician or OB/GYN. Some studies have suggested that it may be more difficult to detect early breast cancer on routine mammography, and for this reason an MRI (magnetic resonance imaging) may be recommended by your physician when there is any doubt about the results of your mammographic evaluation.
What are the Risks of Breast Augmentation?
As is the case in all surgery, there are certain risks that are inherent with this operation. Although the scars are usually well hidden, irregularity or thickening of scars can occur which might require revision.
Rarely, bleeding (hemorrhage) may result due to the trauma of the surgery. Small amounts of blood can be easily managed and broken down by the body; however, a large amount of blood or persistent bleeding often requires a return to the operating room for achievement of hemostasis (stopping bleeding) and wash out of the implant space.
Infection is also a risk with breast augmentation surgery. If an infection occurs, antibiotics may used for a superficial skin infection. However, deeper infections and ones that may be in communication with the implant space may require implant removal. While implant salvage has been described in the literature, there is a reported failure rate of 20-40%. If the patient is a candidate for salvage of the existing implant, this will be discussed with you by your surgeon. If the implant is removed, it will often be necessary to leave the implant out for a period of approximately 3-6 months. At that time a new implants can be placed back in the breast. The risk of infection during the first year, as reported by the manufacturer, is between 0.5 and 1%. While infection is usually confined to the first few weeks after surgery, certain bacteria can show up later and produce infection at a date further removed from surgery.
Another potentially serious complication is implant rejection. Silicone is the least reactive material used for implant construction. Most patients tolerate the material without difficulty. Nevertheless, a very small percentage will react to the implant and require removal to avoid long term sequelae.
Will I Lose Sensation In My Breasts After Augmentation?
Sensory changes can occur resulting in numbness or discomfort, and while these symptoms are usually not long-standing or severe, they can be in some cases. Temporary sensory changes are common and usually last 3 to 6 months. Risk of permanent sensory loss increases with increased implant size since larger implants stretch the sensory nerves further. Implants could possibly interfere with nursing although many patients nurse after the operation without difficulty.
What is Capsular Contracture and how is it treated?
One problem that can occur with any implant placed is the formation of a scar tissue capsule around the implant. As the body recognizes that the implant is not yours, it will naturally try to wall off the implant using scar tissue. In some people, this formation of scar tissue is exaggerated and can form thick scar tissue/capsule within the body. If this occurs, it can cause an unnatural firming of the breast and can even cause breast distortion and pain. This condition is referred to as “capsular contracture.”
In mild cases, breast compression exercises may allow the capsule to stretch and soften. Also, your surgeon may prescribe medications to retard the process of capsular contracture and help to soften the breast. While use of mediations for this purpose (such as Accolate), may be helpful, there is not a guarantee of 100% that the capsule will be softened. Furthermore, there are risks associated with this and similar medications. Your doctor will go over these risks if you are prescribed leukotriene inhibitors such as Accolate for your capsular contracture. More advanced cases, or those that are recalcitrant to treatment, may require further surgery and possible replacement of the implant.
Studies presented to the FDA indicate that the overall risk of requiring further surgery in cases of capsular contracture can be as high as 15 to 20% within the first three years following surgery. If surgery is needed, there are two primary options available: capsulotomy and capsulectomy. Capsulotomy is a simple procedure that works well for mild capsular contracture, but may be inadequate for more severe scar thickening. For more severe capsular contracture a complete capsulectomy (removal of all scar tissue) and replacement of the implant may be required. Unfortunately, there is no certainty that the scar tissue will not reform.
What Causes Rippling after Breast Augmentation?
Rippling, or surface irregularities over the implant that can be seen or felt, is a potential problem with any type of breast implant. It occurs more frequently with saline filled implants because the water in the implant is less viscous than silicone gel. Because of the potential problem, placement of the saline filled implant under the muscle may be indicated to help decrease the risk of rippling. This is because it gives more soft tissue coverage over the implant. This may be particularly true for patients who have very little breast tissue. Since the pectoralis muscle only covers the upper portion of the implant, rippling can still occur where there is not muscle coverage. The bulk and size of the pectoralis muscle varies from individual to individual, and so there is no set rule as to how much of the implant will be protected. A major factor influencing the possibility of rippling is implant size. Larger breast implants tend to stretch and thin out the overlying tissue resulting in less natural coverage over the implant. For that reason, rippling is more common in patients who select very large implants. This is a factor to be taken into consideration when selecting implant size. Implant texturing may also increase the chance and severity of rippling. Smooth surface implants seem to have less of a chance for rippling than textured surface implants. In the event that rippling is noted, an implant can be moved to a deeper position with more tissue coverage. If inadequate tissue coverage exists, the use of dermal matrix (skin substitute) can be used to create coverage of an implant.
How Do I know what size is best for me?
The shape of your augmented breasts depends on the implant size and shape chosen along with how your breast appears prior to surgery. The same size and shaped implant on one patient can look completely different on someone else. Therefore, one should avoid picking a size or shape solely on what ‘looks good’ on someone else.
Implants may be round or teardrop-shaped (anatomical). While teardrop (anatomical implants) may seem like a good idea they have some drawbacks. Teardrop implant widths are different than their length and any rotation may produce an unwanted asymmetry. Round breast implants are the same diameter all around but not ball shaped. Our preference is to use round shaped gel and saline filled implants as they provide excellent aesthetic results without the risk of rotation.
During your consultation our surgeons and nurses will with help you determine the implant size by placing actual filled implants of various sizes in special surgical bras to help estimate the size you desire. You may want to bring different shirts to see how your new look appears in different clothing. Some women find it effective to pad a bra by using baggies filled with birdseed or rice to estimate the approximate additional volume they desire. The final decision is yours but we are always ready to discuss concerns of implant style, shape, and size.
Submuscular or Subglandular Implant Placement?
The breast normally sits on top of the pectoralis muscle. Breast implants can be placed above or below this muscle. When implants are placed below the muscle, it is called a submuscular placement or a subpectoral placement. When the breast implant is placed above the muscle, it is called a subglandular or submammary placement, meaning that it’s below the mammary gland.
We generally prefer to place breast implants below the pectoral muscle. A possible advantage of submuscular placement is that it may allow better mammography and thus less chance of missing a breast lesion. Another advantage of submuscular placement is that the implant is entirely beneath the breast tissue, decreasing the possibility of interference with breast function. Research indicates that implants placed below the muscle are less likely to develop firmness (capsular contracture). This may be the result of pressure or internal massage of the implant by muscle movement. Lastly, placement of the implant below the muscle allows for better camouflage of the implant as there is more tissue covering it.
The primary disadvantage of submuscular implant placement is a slightly more painful and prolonged recovery compared to subglandular placement. The most severe pain lasts for one week on average due to the stretching of the muscle. Another disadvantage is the so called “flexion deformity.” Placement of an implant under the muscle can at times result in a temporary crease along the edge of the muscle over the lower portion of the implant. While noticeable briefly it is of no major concern and the breast appears normal at all other times.
What can I expect for my recovery after breast augmentation?
Anesthesia is provided by a registered nurse if having a procedure under sedation or by an anesthesiologist. Immediately after the surgery, a nurse will monitor you and ensure that you are doing well after anesthesia prior to discharge home on the day of surgery. A layer of elastic tape will be used for 7 days to help support the breast along with a light compression bra. Patients usually return to light activity within two to three days after surgery. Full activity is resumed within two or three weeks but no vigorous bouncing type activities (jogging or horseback riding) is recommended for 4-6 weeks. Although the breasts usually look good almost immediately after surgery, there is an improvement in the shape over the following several months as the inflammation goes down and the implants settle into position.
